Image of the month
How to adjust potassium citrate to minimize calcium oxalate
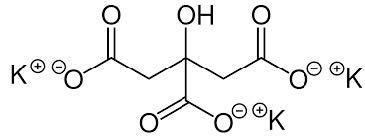
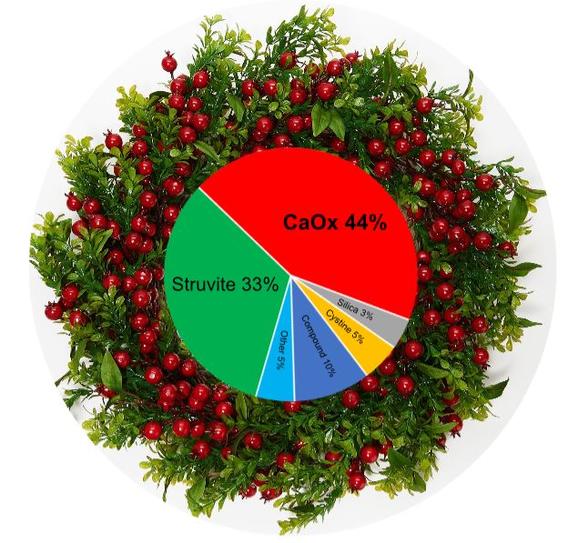
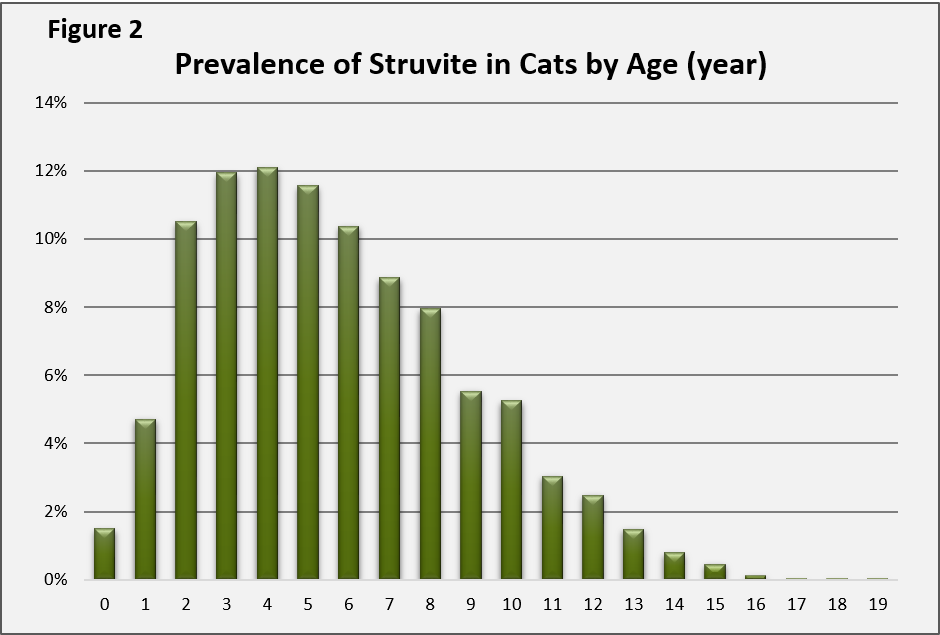
The prevalence of calcium oxalate (CaOx) stones rapidly increased following the implementation of acidifying diets to prevent struvite stones. Potassium citrate, which increases urine citrate and urine pH could reverse this trend. Citrate binds calcium, reducing the amount of calcium available to bind with oxalate.
Citrate reduces CaOx crystal aggregation and aids other crystallization inhibitors. Alkaline urine reduces urine calcium excretion.
Our goal
Potassium citrate is most beneficial in CaOx stone-forming animals with consistently low urine pH ( ≤ 6). Our starting dose is 75mg/kg twice a day to reach a urine pH close to 6.5. Many forms are available. Avoid forms containing cranberries, which are a source of oxalate.
How to adjust the dose
Urine citrate is not routinely measured, but urine pH is. Give pet owners pH paper and have them measure urine pH approximately every 5-6 hours for 2 to 3 days. If the average is near 6.5, no dosage change is needed. For lower values (< 6.0), the dose can be increased by 20% until urine pH approaches 6.5. With adverse effects (decreased appetite, serum potassium > 6.2 mmol/L), the dose is reduced by 20%. We are cautious when administering potassium citrate to animals with dehydration, decreased kidney function, diabetes, and hypoadrenocorticism (disease conditions associated with decreased potassium excretion.