Image of the month
Duking out the treatment of struvite/urate urolithiasis
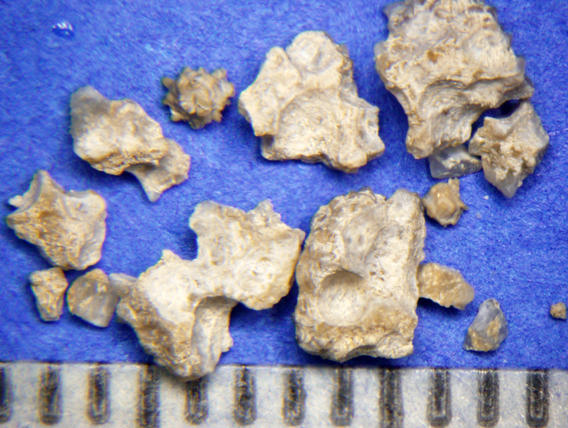
"Duke" is a 12-yr-old MN Shih Tzu presented for intermitted bloody urine. Antibiotics initially resolved clinical signs, but hematuria recurred. Radiographs identified a moderately radiopaque bladder stone (Figure 1). "Duke" was anesthetized, the stone was fragmented by laser lithotripsy (video 1), and the fragments were removed by basket retrieval and voiding urohydropropulsion. Quantitative analysis of the stone was 70% struvite and 30% urate (Figure 2). Taking a second look at the radiograph, liver size was normal but small. Serum concentrations of liver enzymes were unremarkable: ALP = 28 U/L (normal = 22-92), AST U/L = 22 (normal = 16-44) and ALP U/L = 25 (normal = 8 to 139).
How would you manage this dog?

Diagnostically
- Shih Tzu's are predisposed to porto-vascular shunts. Consider evaluating bile acids in breeds at risk for liver shunts. Postprandial serum bile acid concentration was high (52 µmol/L; normal is 15 to 25).
- Culture urine, struvite uroliths in dogs are usually due to a urinary tract infection.
Therapeutically
- To prevent urate, consider canned lower purine/protein foods usually formulated with egg, dairy, or vegetable proteins that result in a more neutral or alkaline urine pH (e.g. Hill's l/d, u/d, i/d Sensitive Canine, HA Hydrolyzed, others).
- To prevent struvite, control urinary tract infection with periodic urine cultures and appropriate antimicrobics, when needed.
If bile acids were normal, we would still avoid urine acidification (a common feature of struvitolytic diets) because urate is more soluble in alkaline urine and therefore less likely to precipitate out.
Additional resources
- Read more in depth recommendations to prevent canine struvite/urate uroliths (PDF)
- Watch videos of voiding urohydropropulsion
- Use of urohydropropulsion, cystoscopy and lithotripsy to manage feline urolithiasis, Jody Lulich DVM, PhD, DACVIM, Hill's Global Symposium on Feline Lower Urinary Tract Health, Prague, 23rd - 24th April 2014 Voiding urohydropropulsion. Lessons from 5 years of experience. Lulich, JP, et al, Vet Clin North Am Small Anim Pract. 1999 Jan;29(1):283-91, xiv.
Image of the month
The rings of Saturn
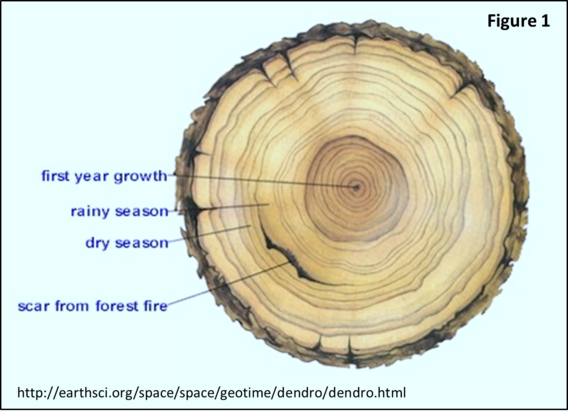
Tree-ring dating, dendrochronology, is the study of climate and environmental changes as recorded by the growth rings of a tree. These concentric rings can be wide, indicating a wet season of rapid growth, narrow indicating a dry season of slow growth, or blemished, indicating fire or insect damage (Figure 1).
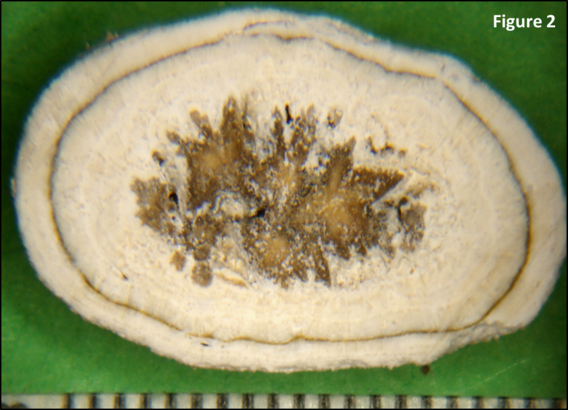
A similar analogy, urochronology, can be used to tell the life-story of uroliths. Figure 2 is a urolith from Saturn, a female/spayed, Jack Russell terrier. The center or origin of the urolith is calcium oxalate indicating excessive urinary calcium excretion (hypercalciuria) resulting from metabolic, genetic, dietary or idiopathic causes. The white layer is struvite indicating urinary tract infection caused by urease producing bacteria. Staphylococcus and Proteus spp. are common examples. Next, a dark narrow band of calcium oxalate is repeated indicating a period of antibiotic clearance of bacteria but without control of hypercalciuria. Finally, the struvite returns in the outer layer because antibiotics were prematurely stopped.

Figure 3 is a bladder stone from a female Labrador retriever. The center is composed of calcium phosphate carbonate and the remaining outer layers are struvite. Both minerals are infection induced. The wide layers likely represent periods of rapid growth and the narrow layers are periods of slower growth. Reading the layers of bladder stones provide a glimpse into the climate in the urinary tract during formation. This story of urochronology can help determine therapy needed to minimize recurrence.
For additional information see our Canine Compound Urolith Recommendations.
Image of the month
It's a small world after all - global calcium oxalate
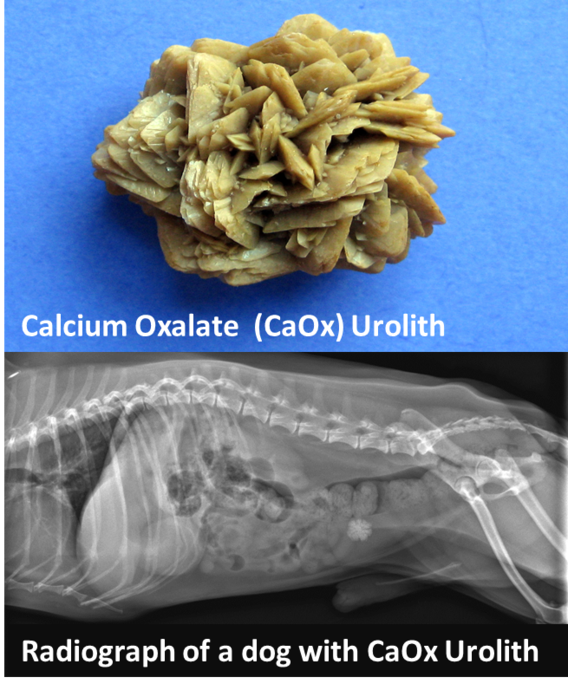
Globally, calcium oxalate (CaOx) is the most frequent urinary stone affecting dogs. The positive health implications of early recognition of CaOx stones include nonsurgical removal, early dietary modification to minimize urolith growth, and early removal to avoid urinary obstruction. To achieve these health benefits, CaOx urinary stones need to be recognized early prior to the development of clinical disease. We can help. Males are affected more than females. Around the world the most common breeds that form calcium oxalate are the Maltese, miniature Schnauzer, Shih Tzu, Yorkshire terrier, and Chihuahua. The most common age for the onset of clinical disease is 7 to 8 years. We recommend to begin screening (i.e. medical imaging) high risk dogs at 5 to 6 years of age.
View the list of the top 10 canine calcium oxalate forming breeds by continent.
To look up the risk of CaOx stones in other breeds, download our App (MN Urolith from the AppleStore for iPhone and iPad or Minnesota Urolith Center Google App for Android.
Minnesota Urolith Center CALCulator function demo
Image of the month
It's a small world after all - global canine struvite

In 2017, the Minnesota Urolith Center analyzed Magnesium Ammonium Phosphate (struvite) stones from over 26,000 dogs that could have been dissolved with therapeutic food and antibiotics.
How can you determine if stones are struvite before their removal and analysis? Around the world the most common breeds that form struvite are the miniature Schnauzer, Shih Tzu, Pug, Yorkshire terrier, Dachshund, miniature Poodle and Bichon. View the list of top 10 canine struvite forming breeds by continent (PDF). Although these are the same breeds that form calcium oxalate, the difference is that 85% of dogs that form struvite are female, most calcium oxalate stone formers are male. With struvite, urine pH is often alkaline, while urine is often acidic with calcium oxalate.
Want to dissolve struvite? Therapeutic food and antibiotics need to be administered throughout the entire period of dissolution (2 to 3 months). View our Canine Struvite Urolith Recommendations - Medical dissolution of struvite page (PDF) and video below. Six to 8 weeks after initiating therapy, recheck a lateral radiograph. If uroliths are smaller, continue therapy until stones are gone. If urolith size and density have not changed, the stones may not be struvite. Consider removal and submit uroliths for mineral analysis.
Use the CALCulate function on our App to help predict mineral composition based on breed, gender and age. Download our App MN Urolith from the AppleStore for iPhone and iPad or Minnesota Urolith Center Google App for Android. See CALCulate function video demo.
Image of the month
Cystine rising: Ferreting out the cause
Cystine rising: Ferreting out the cause
Cystine (also called dicysteine) is a dimer of two sulfur-containing amino acids of cysteine. Cystine is sparingly soluble in urine and efficiently reabsorbed by kidney tubules. However, genetic mutations in the cystine transporter inhibit the kidney from reabsorbing cystine. Genetic mutations have been identified in dogs, cats and humans with cystine uroliths.
What about cystine in ferrets

(Figure 1 and 2) Initially, we reported that the most common urinary stone in ferrets was struvite, 67% of 408 submissions received between 1981 and 2007 (Figure 3). The second most common urolith was cystine (15%). Over the last 8 years, the tables have turned. From 2010 to 2017, only 6.5% of the 700 ferret urolith submissions were struvite, and a whopping 89% were cystine. (Figure 4)

Help us ferret out the reason why
The Minnesota Urolith Center and the U of MN Canine Genetics Lab are investigating genetic mutations responsible for cystinuria in ferrets. Genetic screening is performed at no cost to you (USA cases only). Contact Dr. Furrow at the Canine Genetics Laboratory for genetic testing.
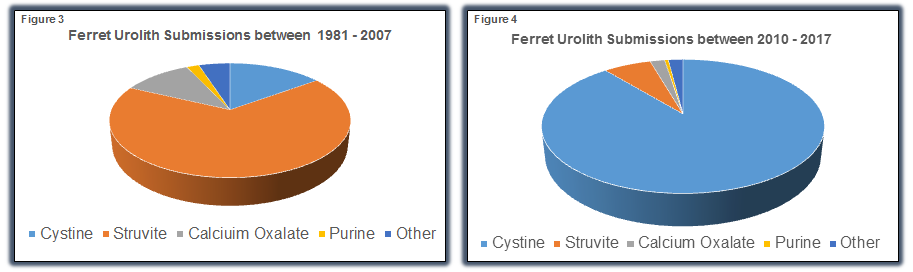
Image of the month
Being crystal clear about crystalluria
Crystals only form in urine that is supersaturated with lithogenic substances. Therefore, crystalluria represents a risk factor for urolith formation. Crystalluria can aid prediction of urolith composition, serve as a marker for undiagnosed disease (e.g. urate crystals in dogs with protovascular shunts), and index therapy effectiveness (e.g. castration to resolve cystinuria).
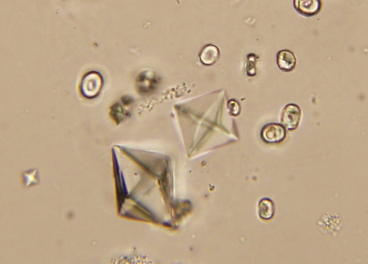
Crystalluria (or lack thereof) should never be used as the sole indicator for urolith disease. Here are reasons why:
- Uroliths can be present without crystals.
- Crystals can be present without uroliths.
- Increases in urine pH favor struvite crystals even in dogs and cats with non‐struvite stones.
- Once uroliths form, crystalluria lessens in severity or disappears; this is because less energy is needed to attach minerals to preformed uroliths (stone growth) than to precipitate to form new crystals.
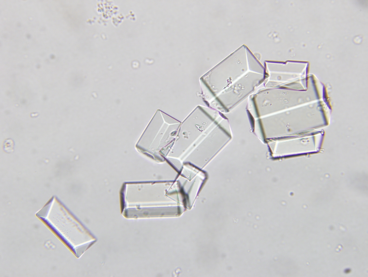
Although crystalluria is proof that urine is supersaturated with lithogenic substances and a risk for urolith formation, care must be used to not over‐interpret the significance of crystalluria in urine samples that are:
- collected by owners
- refrigerated prior to analysis
- sent out to laboratories for analysis
- analyzed more than 30 minutes to 2 hours after collection

In vitro changes may not represent in vivo conditions. Therefore, analyze urine in your clinic as soon as feasible after collection to achieve the most reliable results.
Image of the month
Common questions on dogs forming cystine stones
How will I know if my dog has cystinuria?
- Cystine is an amino acid that is freely filtered in urine and almost completely reabsorbed by the kidney tubules (i.e. removed from the urine).
- As urine cystine concentration increases, a positive urine nitroprusside test, cystine crystals and cystine stones are indicators of disease.
- Although cystinuria and cystine crystalluria do not cause clinical signs, cystine stones can irritate the lining of the urinary tract resulting in urinary accidents, urgency, straining, or bloody urine. In some cases, the stones result in life-threatening urinary obstruction. Cystine stones are not always visible on x-rays and may require special contrast studies or an ultrasound to diagnosis.
- Genetic tests for cystinuria are available for some breeds of dogs. A genetic marker test for androgen dependent cystinuria has been developed for Mastiffs, English bulldogs and French bulldogs. There are other breeds with androgen dependent cystinuria as well as other breeds in which castration will not reduce cystinuria (Type Ia, reported in Newfoundland dogs, Labradors and Landseers,Type IIa, reported in Australian Cattle dogs and Border Collies, Type IIb, reported in Miniature Pinschers).
Will castration prevent recurrence of cystine stones?
- Surgical or medical castration can resolve/cure cystinuria in the subset of male dogs with androgen dependent cystinuria.
- The magnitude of cystinuria associated with stone formation is wide (100 to >10,000 ɥmol/g creatinine) and varies between serial measurements in the same dog. This emphasizes that other factors such as diet, urine specific gravity and urine pH influence stone formation.
- To determine if castration reduces cystinuria, measure urine cystine (cystine/creatinine ratio) before and 3 months after castration. Reference ranges are under development; consider serial monitoring looking for a decreasing trend. Undetectable levels may indicate resolution of cystinuria. If the urine cystine remains elevated at 3 months, check again at 6 months. If the test is persistently positive, it indicates that the dog has a non-androgen dependent form of the disease. These cases are at risk for recurrence without additional therapy. Less sensitive indicators of urine cystine that can be evaluated before and after castration include urinalyses for cystine crystalluria, and recurrence of small stones.
Is a negative nitroprusside test following castration an indication that your dog will not reform stones?
- Possibly, but not for certain.
- The nitroprusside test is a qualitative screening test for disease (quantitative tests are better).
- Some dogs with cystinuria are negative on this test even though they have the disease. If the nitroprusside test was only evaluated after castration, it is difficult to determine if castration reduced cystine excretion. In this situation, measure urine cystine concentration. In most stone-free dogs, cystine concentrations are extremely low.
- Studies on human urine indicate that the nitroprusside test is influenced by urine specific gravity and creatinine, but not by thiola or D-penicillamine. Ampicillin and sulfur containing drugs have been reported to cause false positive results. This test may also be influenced by ascorbic acid, which dogs are able to synthesize within their body (unlike people). Therefore, the accuracy of this test in dogs should be interpreted with this in mind.
What diets prevent cystine stones?
- A 25% reduction in 24-hour urine cystine was associated with consumption of Hill’s Prescription diet u/d.
- Avoid diets that promote formation of acidic and concentrated urine, which are risk factors for stone formation.
- Diets rich in methionine (a precursor of cysteine and a common amino acid in animal protein sources) may contribute to cystine recurrence. Consider lower protein foods with reduced quantities of animal protein.
- Studies in cystinuric humans suggest that dietary sodium enhances cystinuria, and therefore high sodium diets (>100-150 mg/Kcal) should be avoided.
Additional cystine resources
- Osborne et al. Canine cystine urolithiasis: cause, detection, treatment….. VCNA. 1999;29:193
- Chillaron, J. et al. Pathophysiology and treatment of cystinuria. Nat. Rev. Nephrol. 2010:6;424-434
- Brons et. al. SLC3A1 and SLC7A9 mutations in….canine cystinuria. JVIM 2013;27:1400.
- Brady et al. Cyanide-Nitroprusside Colorimetric Assay: a rapid colorimetric screen…... JALM. 2017;2:55
- Thiola® (Tiopronin, 2-MPG )
- Effective September 2014, Thiola is no longer distributed by Mission Pharmacal.
- Thiola is available directly from the distributor Retrophin at: thiola.com phone: 844-4-THIOLA (844-484-4652)
- Tiopronin tablets are available through compounding pharmacies. Contact your preferred compounding pharmacy for availability. One pharmacy we have identified that offers compounded capsules and suspensions (confirmed availability: June 2016) Wedgewood Pharmacy phone: 877-357-6613
Alternatives
- L-cystine methyl esters - Studies in the mouse model have shown that these compounds are effective in disrupting cystine crystal growth. Future studies hope to show that efficacy and safety profiles are superior to current thiol-binding drugs. Sahota, A: Novel Cystine Ester Mimics for the Treatment of Cystinuria-induced Urolithiasis in a Knockout Mouse Model: UROLOGY 84: 1249.e9e1249.e15, 2014
- Cuprimine® D-Penicillamine - D-penicillamine,c also called dimethylcysteine, is a first-generation cysteine chelating drug. Although D-penicillamine is effective in reducing urine cystine concentrations, drug-related adverse events limit its use. Therefore, we have discontinued using D-Penicillamine for cystinuric dogs and cats.
Additional information regarding cystine urolithiasis
- Minnesota Urolith Center's treatment recommendations
- Osborne C, et al: Canine Cystine Urolithiasis: Causes, Detection, Dissolution, and Prevention: Small Animal Clinical Nutrition 5, Mark Morris Institute http://bookstore.markmorrisinstitute.org/ (download at no cost)
Resources for cystinuria testing (urine nitroprusside/genetic testing/metabolic screening)
- PennGen Laboratories - http://research.vet.upenn.edu/penngen
Resources for Urine Amino Acid Testing
- UC Davis Amino Acid Laboratory - www.vetmed.ucdavis .edu/labs/amino-acid-laboratory
Image of the month
Dissolving feline struvite stones
Dissolving feline struvite stones
Struvite is the most common feline stone analyzed by the Minnesota Urolith Center. Diet has played an important role in struvite dissolution and prevention for over 35 years. Dry and canned therapeutic foods are 100% effective in dissolving feline struvite uroliths in about 1 to 3 weeks.
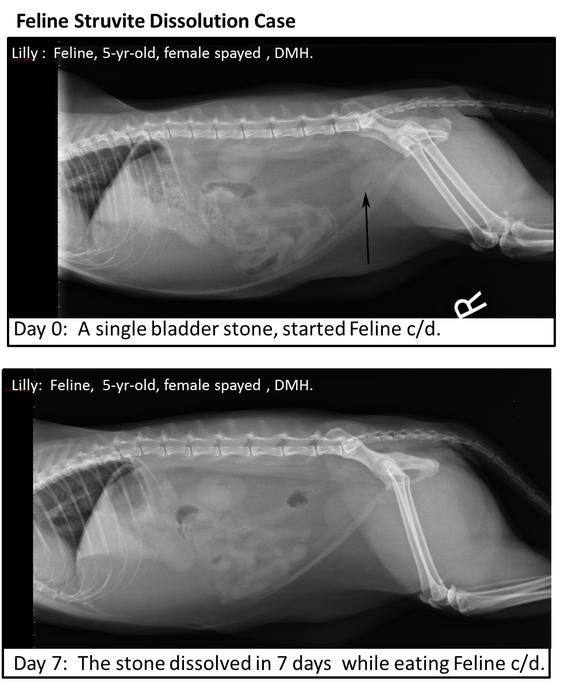
The case of Lilly a 5-yr-old, female spayed DMH presenting with dysuria and hematuria. The urinalysis did not reveal crystalluria.
Radiography at Day 0 revealed one marginally radiopaque bladder stone consistent with a composition of Struvite.
Repeat radiograph at Day 7 showed the stone had dissolved in 7 days while eating Feline c/d diet.
Protocol for dissolving feline struvite uroliths (*ref)
- Start nutritional therapy.
- Repeat radiographs in 2 to 3 weeks.
If the stones are smaller, continue nutritional dissolution. Repeat radiographs in 2-4 weeks. If the stones have completely dissolved initiate Feline Struvite Prevention.
If stones are not smaller, re-evaluate diagnostic information to confirm stones are struvite (use CALCulator function on the MUC App).
Reasons why stones are not smaller
- Stones may not be struvite; consider other removal strategies
- Stones are associated with a urease urinary tract infection. Culture urine and administer antibiotics with diet to dissolve stones.
- The cat is not eating the prescribed food. Select a different flavor/formulation or consider a gradual food transition. Remind owners of the rapid success with diet compliance.
Common Questions?
Is Urethral Obstruction likely when dissolving struvite stones in male cats?
No. The truth: In published studies on feline struvite dissolution, where approximately 1/3 of cats were male, no cat developed urethral obstruction.
Is Struvite crystalluria the primary method for predicting mineral composition?
No. The truth: Crystalluria occurs in less than 10% of cats with struvite stones. Radiographs in conjunction with the CALCulator function, on the MUC App, are the most accurate tools to predict mineral composition.
*Ref - Efficacy of two commercially available, low-magnesium, urine-acidifying dry foods for the dissolution of struvite uroliths in cats. Lulich JP, Kruger JM, Macleay JM, Merrils JM, PaetauRobinson I, Albasan H, Osborne CA. J Am Vet Med Assoc 2013, Oct 15:243(8); 1147-53.