Leading the resistance—against antimicrobial resistance
July 16, 2024
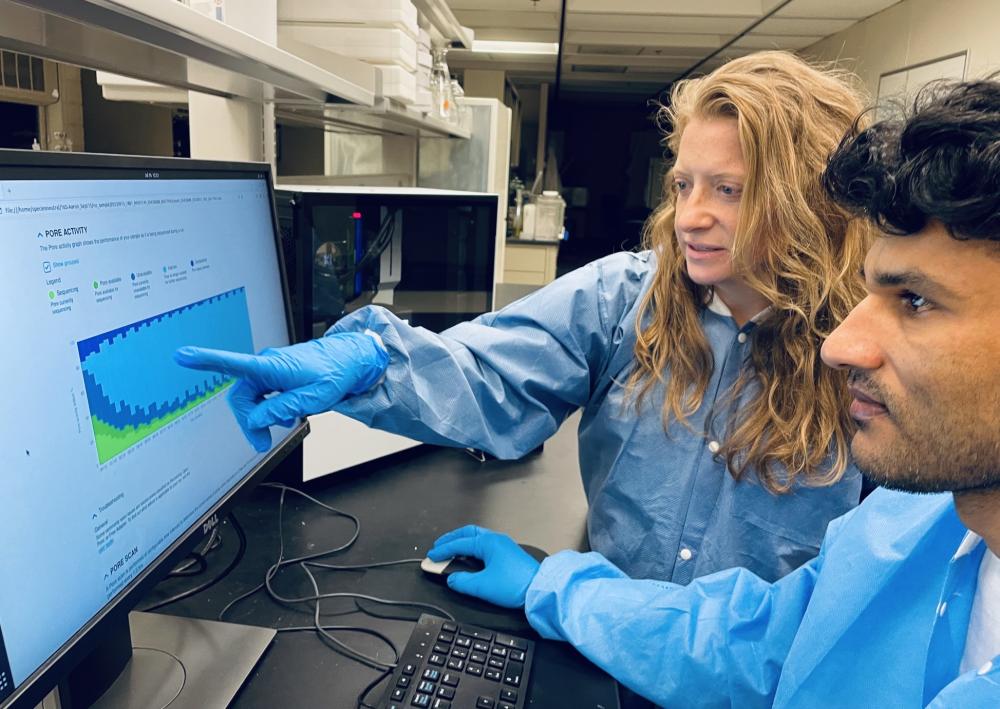
Noelle Noyes and postdoctoral fellow Tara Gaire review data produced by the TELSeq workflow.
Noelle Noyes, Associate Professor at the College of Veterinary Medicine, has received a 5-year, $3.6 million grant from the National Institutes of Health Institute of Allergy and Infectious Disease to develop an important new tool for combating antimicrobial resistance. Her team is taking a novel approach to understanding the genetics behind antimicrobial resistance, an approach that could have significant practical applications for patient treatment and public health.
Antimicrobial resistance (AMR), which the World Health Organization has identified as one of the greatest global public health threats, causes millions of deaths every year. Microbes such as bacteria can adapt over time at the genetic level to develop resistance to the medicines designed to treat bacterial infections. This resistance can render those antimicrobial treatments (such as antibiotics) ineffective, so that even common infections and minor injuries can become deadly.
Many efforts have been made to reduce resistance, but despite these efforts, resistant pathogens continue to emerge and persist. This is in part because bacteria acquire AMR genes in ways that are complex—and poorly understood. Without better information about the basic mechanisms that drive resistance, doctors’ ability to make predictions about resistant infections—and therefore to prevent and treat them—is hampered.
Noyes hopes that her project will ultimately decrease AMR-related complications and deaths by advancing knowledge of how AMR genes behave.
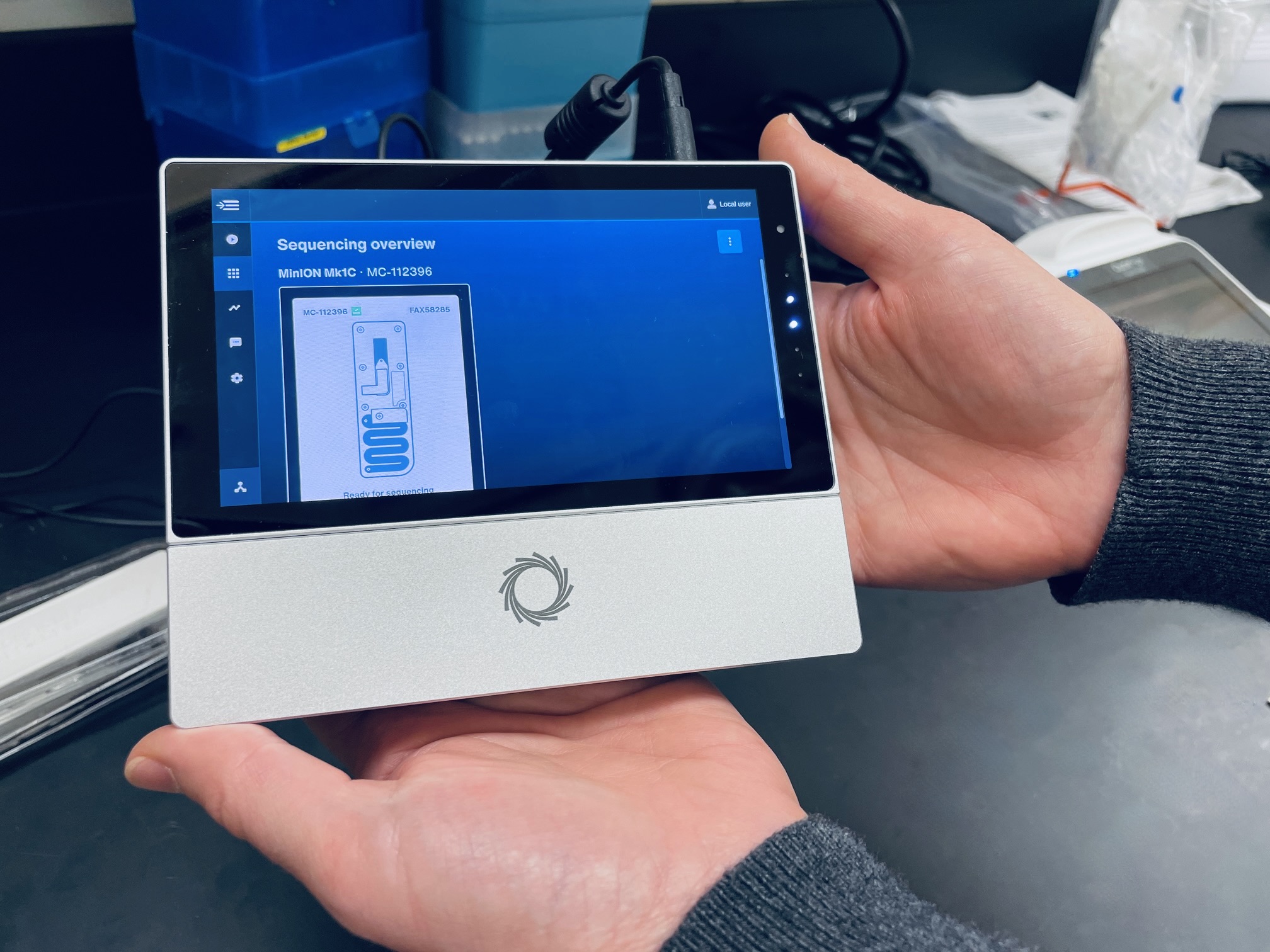
Her team is refining a new approach to generating highly accurate and detailed genetic data called target-enriched long-read sequencing (“TELSeq”), along with methods that will make the generated data easily accessible and guidance for scenarios where the data can be used. “While we’ve been using this method for a few years now for research purposes, it remains to be seen how versatile and repeatable the method is with different types of samples and under different settings,” Noyes described. “These are big considerations for moving tools beyond purely research, and I’m excited that we’ve received robust funding to test the limits of the technology.”
Their approach will open new opportunities for foundational research and hopefully offer improved information for patient treatment and public health decision-making. This means predicting AMR emergence in patients and populations; identifying hot-spots of AMR development and spread in hospitals and the community; and helping to track important AMR genes that are critical for future research.
“The thing that excites me most about this project is that we get to dive super deep into new data, generated using a relatively new method,” Noyes said. “This could mean big potential for scientific discovery, and I just love that process of sitting in front of a brand new dataset, and asking it to reveal its secrets. Sometimes there’s not much there, and that’s okay—that’s the process of science. But sometimes, you find something new and interesting, and that is really exciting to me. That’s the best part of my job.”


