CVM researchers test less invasive imaging techniques for understanding development of Legg-Calvé-Perthes disease
December 13, 2023
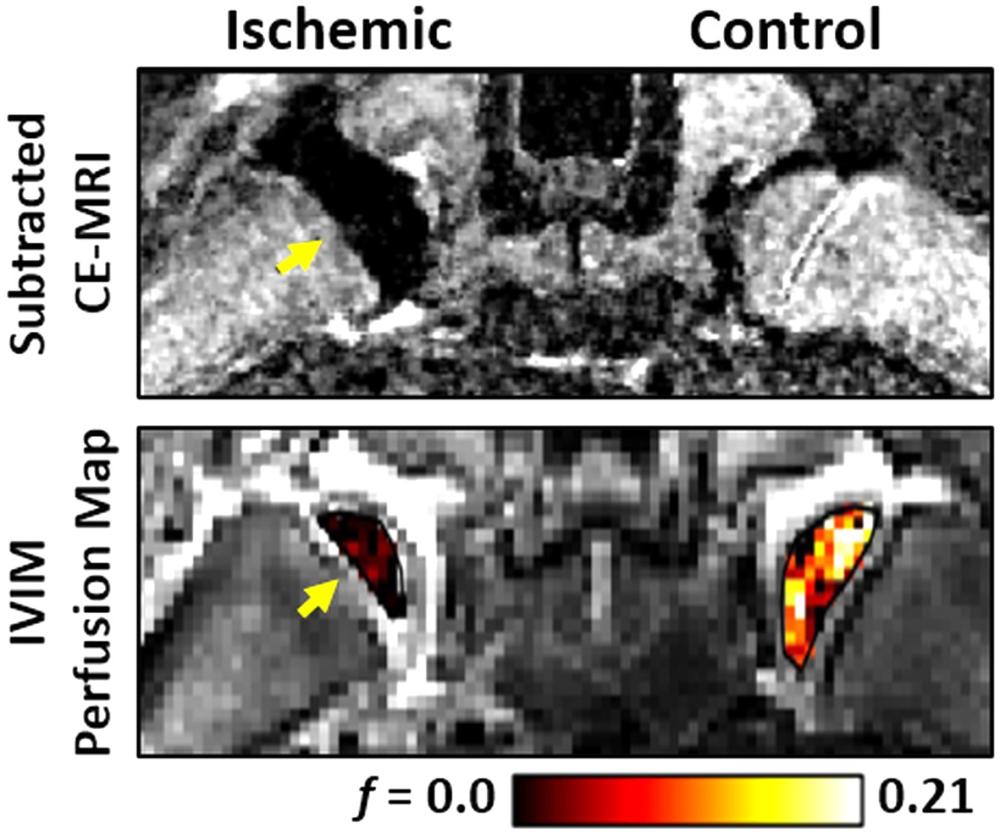
Example images of the femoral heads of a piglet model of LCPD using the conventional, contrast-enhanced MRI approach (top) and the new, non-contrast-enhanced IVIM approach (bottom). The femoral head lacking blood flow (yellow arrow) appears dark compared to the contralateral, perfused femoral head.
A team of researchers led by Casey Johnson, assistant professor of medical imaging at the College of Veterinary Medicine, and postdoctoral researcher Erick Buko, are studying less invasive imaging techniques for early detection and assessment of a rare but debilitating disease, called Legg-Calvé-Perthes disease (LCPD). LCPD, which primarily affects children and adolescents, is a condition in which the ball-shaped head of the hip joint (femoral head) has a temporary loss or disruption of its blood supply. As a result, the femoral head can become deformed and fracture. LCPD can lead to the onset of hip osteoarthritis and can even require hip replacement at a young age.
Treatment for LCPD often consists of procedures aimed at restoring blood flow to the area, and eventually formation of new bone, in an effort to restore the head of the femur. Surgical interventions can also speed up this repair process. A crucial aspect of the decision-making process for treating LCPD is the perfusion (blood flow) status of the femoral head, as this informs the severity and stage of the disease, as well as determining whether surgery will be necessary for treatment.
Currently, the primary method used to clinically assess the severity and status of LCPD in its earliest stage is subtraction contrast-enhanced magnetic resonance imaging (CE-MRI), using an intravenous injection of a contrast agent material. However, due to uncertainty around the potential long-term effects of contrast agent in pediatric patients, coupled with the need to sedate children in order to obtain high-quality results, this method is used sparingly. This means there is a significant need for an alternative method to assess femoral head perfusion in LCPD patients. A non-contrast method would enable more frequent MRIs, which would both inform treatment decisions, and also lead to a better understanding of the potential causes and contributors to LCPD as a whole.
This is where Johnson, Buko, and their collaborators come in. Their proposed alternative method is called intravoxel incoherent motion (IVIM). IVIM is a non-contrast-enhanced MRI technique that uses a multi-pronged method to measure the tissue damage and perfusion severity. IVIM has been used for similar purposes with tissues such as the brain, liver, pancreas, kidney, and prostate. But tissues like bone marrow present some challenges to the IVIM method, so the method needs to be further validated and improved upon to image bone marrow blood flow (perfusion and ischemia).
The purpose of this study was to determine if IVIM can detect femoral head ischemia (inadequate blood flow) using a piglet model of LCPD, with CE-MRI as the gold standard. The study’s findings show that the new, less invasive IVIM method is effective in detecting a decrease in bone marrow blood flow in young femoral heads without the use of a contrast agent injection. IVIM can also measure an increase in water diffusion, a commonly known result of ischemic femoral head injuries. It was therefore found that IVIM can assess both the blood flow status and severity of femoral head injuries. These findings support that IVIM may be a suitable non-contrast-enhanced approach for early detection and monitoring of LCPD to inform treatment decisions.
While these findings demonstrate the capabilities of IVIM to detect ischemia and perfusion of the femoral head, there are technical challenges that need to be addressed before this technique can be used clinically. These challenges can require longer scan times, which may not be suitable for imaging pediatric patients. Therefore, further technical improvements are likely needed to make using IVIM in pediatric patients with LCPD feasible. “Our study provides an important validation of the IVIM technique to measure bone marrow ischemia and perfusion,” says Johnson. “We are now working to build upon this work to make the method practical for imaging of children with LCPD to provide a critical window into the disease process to help inform clinical management and treatment of this complex hip disorder.” Read the full study findings in the Journal of Orthopaedic Research.


